Fly the line long enough and chances are you’ll experience an in-flight medical emergency. They are relatively common, but also inherently challenging – they happen in a complex environment, in a confined space and with limited medical equipment often hours from help.
Just how common?
In approximately 1 per 600 flights. Or if you look at it another way, for every million passengers carried, 24 will have a medical emergency.
That may not seem like a lot but wait til you crunch the numbers. At pre-Covid levels four billion passengers were flying annually which meant at least 260 in-flight medical emergencies were happening each and every day. Other reports suggest the real numbers were much higher.
So it is a risk that we take on every time we launch upwards into the wild blue yonder and yet concerningly one we practice for far less often than almost all other inflight emergencies. It is well worth taking a closer look.
Why do people get so sick at altitude?
One of the most common thoughts we have following an in-flight medical emergency is “but he was totally fine when he boarded...”
The reality is the pressurized cabin of an airplane is a terrible environment for someone experiencing a medical situation.
Passengers with existing conditions are probably not aware of the environment they are entering and the effect that it may have on them. They may feel fit to fly on the ground, but in the sky it can be a whole other ball game.
In most cases we are breathing oxygen equivalent to an elevation of between 5000 and 8000 feet. It’s not dangerous, but even healthy people will be mildly hypoxic with oxygen levels almost ten percent lower than normal. At sea level with similar blood oxygen levels an ER would have you on oxygen. Throw in a heart or lung condition and you have a dangerous combination.
Then there’s the issue of sitting down for hours on end which can inhibit the flow of blood in your veins. This can trigger some truly nasty things such as thrombosis (blood clots) and embolisms which can lead to seizures, strokes and heart attacks.
Then there’s the cabin air itself. Re-circulated air can expose passengers to allergens and potentially anaphylaxis – a life threatening allergic reaction. Ever wonder why peanuts in planes aren’t that common anymore? Even something as simple as dehydration can make a passenger become seriously unwell.

A few innocent peanuts a few rows down can lead to a life-threatening medical emergency.
So which ones are the most common?
Almost half of in-flight medical emergencies are caused by neurological conditions, and the vast majority of those are headaches, fainting or dizziness. In most cases they are not serious but may indicate or lead to something far more dangerous.
In second place are gastric symptoms – yep, stomach problems. Beware the dodgy airport taco. Nausea, vomiting and cramping. No one enjoys ‘riding the porcelain express,’ especially in an airplane, but acute food poisoning can become incapacitating very quickly – and the same applies to crew as well as passengers.
And tied for third are respiratory issues (problems breathing) and cardiovascular symptoms (heart related things).
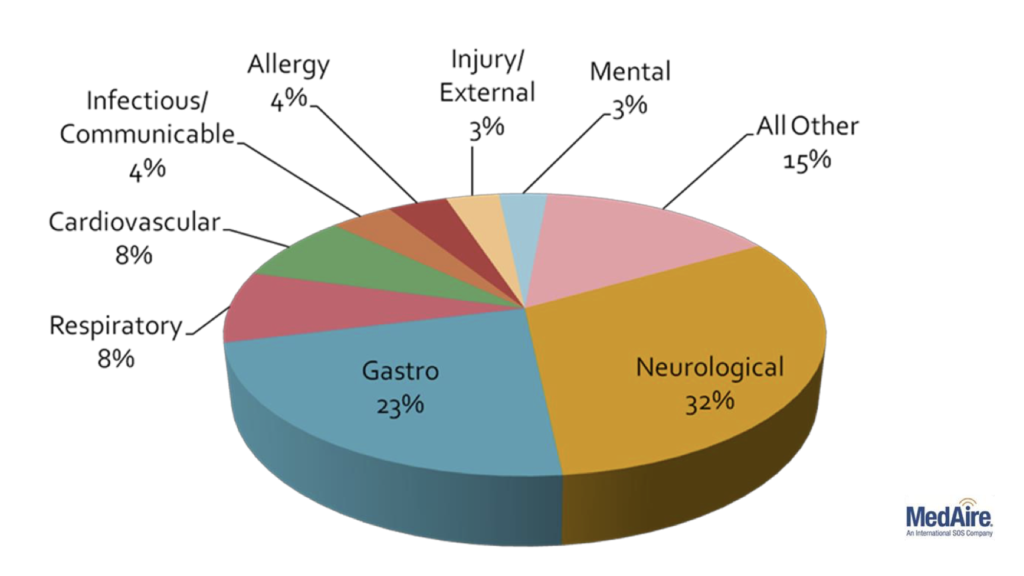
The most common causes of inflight medical emergencies.
Which symptoms do we need to be most worried about?
Human bodies are complex machines but these are historically the biggest warning signs:
- Unconsciousness with slow or no recovery.
- Chest Pain.
- Seizures.
So how do we best manage in-flight medical emergencies?
Prevention is your first line of defence. Don’t board a passenger you have concerns about unless you are completely confident they are fit to fly. This may include speaking to a service like Medlink or asking for medical clearance from a doctor. They may be feeling okay now, but not so much after wheels-up.
Have a plan.
Just like you have a checklist for a mechanical issue in the air, you should have a standard operating procedure for inflight medicals.
Serious health problems often begin with very mild symptoms. Be alert for any medical issues, however minor. A report from the cabin that someone is feeling unwell is your cue to become diversion minded. Start thinking about what is around you, what the weather is doing, and of course those pesky Notams. But the point is: work hard now so if things escalate you are already ahead of the airplane.
Stay calm.
Things are going to get busy but don’t forget that your primary responsibility is to protect your airplane. Remember to fly. If you are multi-crew, make sure one pilot is actively monitoring and has the radios at all times.
Communicate.
This is vitally important. If you plan to use a service like Medlink the first thing they will need is information – and lots of it. Establish communication with the cabin and get that pen and paper out. There are also forms available online to help. Don’t wait until you have the doctor on the line.
Ask for help. You’d be surprised how often you carry passengers with medical experience. In the US they are protected from any liability by the Good Samaritan Law, while in most other countries they have their own provisions which will allow them to assist. Unless they are grossly negligent they simply cannot get in trouble for helping.
Use a medical advisory service. They are invaluable and put you in direct contact with a team of physicians who are trained in ER medicine and airline protocols. They are multi-lingual and available around the clock. They will work with your cabin crew with confident instructions including the use of a physician’s kit. Medlink is a solid example and widely used by carriers around the world. You can contact them via SATPHONE, HF/VHF radio or even ACARS.

Medlink physcians are trained in both ER medicine and airline protocols.
Don’t forget ATC. Don’t be afraid to declare an emergency, or a PAN. They will assist you with priority handling, an ambulance and paramedics on arrival and can even contact your company for you.
Remember security.
It is easy to be distracted during a medical event. Your cabin crew will likely be busy, and you may have to open the flight deck door multiple times. Be aware that medical episodes have previously been used to create a distraction for someone else to try and gain access to the flight deck. Or you may be carrying someone who simply seizes the opportunity. Stick strictly to your security and access procedures.
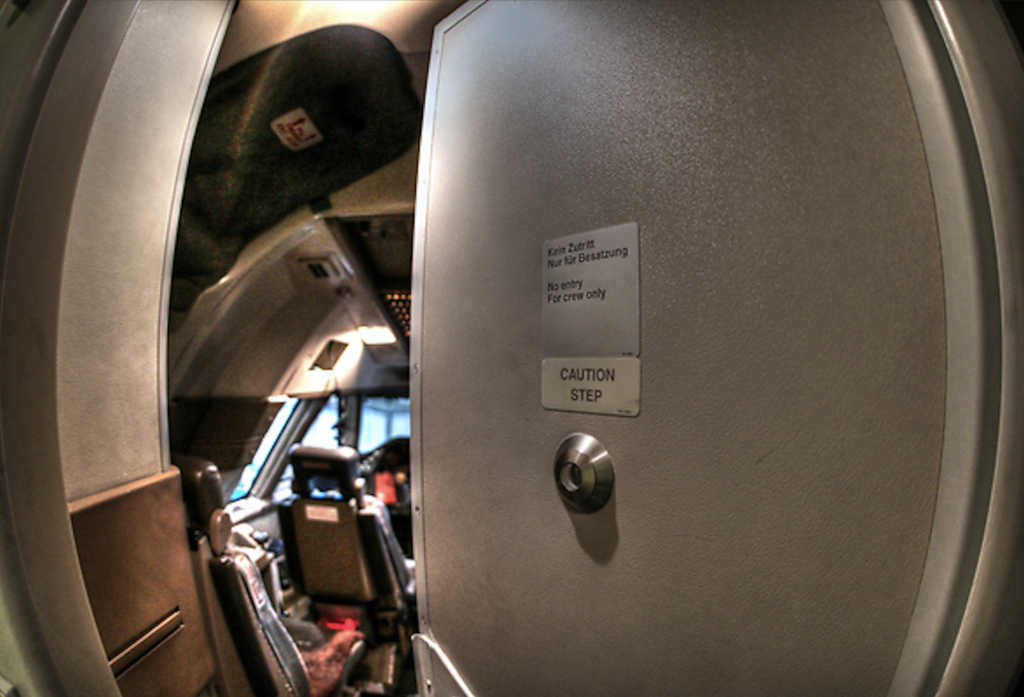
Don’t forget your security – beware of distractions.
Decide. The hard part.
The decision to divert is a complicated one and unfortunately no two situations are the same. But there are a few operational considerations you need to take into account before you hit the old direct-to button.
It’s important to remember medical advice from a service like Medlink is a decision making tool. They cannot make the decision to divert for you – that responsibility sits firmly in the hands of the pilot-in-command.
They can advise you to divert, but remember, they are not aviators. They may not be familiar with the operational risks to you and your passengers of nearby diversion airports. Beware of inherent risks of where you decide to point the nose.
By no means an exhaustive list, but here are some of things you might need to consider above and beyond the emergency on hand:
- Are we over weight? Do we need to dump fuel?
- What’s the current weather? Can we even get in?
- What about terrain? We’re not familiar, are there special procedures?
- Is ATC on watch?
- What about the NOTAMs? Is the runway open?
- Is the runway long enough?
- Is there customs there?
- What do we do when we land? Are there services available?
- Can we gas up there?
- What about the security situation?
You get the picture.
Then there is the standard of medical care. You may give a sick passenger better odds by diverting further afield to land somewhere with better medical response. The closest airport is not always the best one.
And of course cost – the elephant in the room. Some symptoms are clearly life threatening and that must always come before cost. But in other cases it is not always so clear. Professional medical advice does not always take into account the sometimes extreme cost of diverting. For a jet aircraft this can range from $20,000 USD up to $700,000 USD for a large one in logistical costs.

The diversion decision – harder than it looks.
What about illnesses that are contagious?
Now, more than ever before, we are aware of germs. A passenger may suffer a medical emergency because they are carrying something contagious. It is very important that if you suspect a passenger might be infectious that you report it to the right people.
In fact ICAO requires it. If you delve into the depths of ICAO Doc 4444 you’ll find that the pilot-in-command must report to ATC if they suspect they have an infectious passenger on board.
How would you know? ICAO can help with that too. It you have passenger with a temperature greater than 38°C/100°F along with symptoms such as vomiting, coughing, problems breathing, rashes or confusion you can suspect they’re carrying something nasty.
The exact procedures vary from AIP to AIP, but in the US the FAA require pilots to advise either ATC or your company. You can read more about that here.
The problem’s not going away.
Unless you have discovered the ultimate cure for all things medical, in-flight medical emergencies aren’t going away. It is a risk we take every time we take passengers or ourselves into the air. It is up to us to mitigate through knowledge, procedures and preparedness. Chances are when one happens, you won’t be expecting it…
More on the topic:
- More: Out of Options, Out of Time: Why Aren’t We Declaring Emergencies?
- More: Going Viral: The non-Covid nasties to watch out for
- More: Currency and Startle Factor – How to Beat It
- More: US pilots and air traffic controllers can now take the Pfizer vaccine
More reading:
- Latest: NAT CPDLC Route Uplinks: Crew Confusion and Errors
- Latest: Delays and Diversions at TNCM/St Maarten
- Latest: World Cup 2026 Ops Guide – USA, Mexico and Canada
- Safe Airspace: Risk Database
- Weekly Ops Bulletin: Subscribe
- Membership plans: Why join OPSGROUP?











 Get the famous weekly
Get the famous weekly